If you think you are in labor, please call us at 802-371-5961.
We know these are uncertain times, and that you may be apprehensive about important decisions regarding your pregnancy. Please know that we are here for you, ready to support and care for you through your pregnancy, labor and delivery. The CVMC Women’s Health team is taking the necessary precautions to assure babies, mothers, and family members are safe from COVID-19.
To help guide your decisions, members of our healthcare team have developed answers to questions you may have about prenatal care, labor and delivery as they relate to COVID-19.
If I am pregnant, can I work during the COVID-19 pandemic?
You may work while pregnant. If possible, you should work from home. If you must work outside the home, keep a physical distance of 6 feet from other people. Wash your hands frequently. Try not to touch your face. Sanitize surfaces frequently, especially doorknobs.
If you work in health care, you may continue to work by wearing personal protective equipment (PPE) when appropriate. If at all possible, you should avoid taking care of patients known or suspected to have COVID-19, especially during aerosol-generating procedures.
Once you are 37 weeks pregnant, we recommend you stop work outside the home, at which point you should continue physical distancing and quarantine at home.
How will my prenatal care change during the COVID-19 pandemic?
In order to support social distancing, we are trying to decrease the number of in-person prenatal visits. To the extent possible, we will combine office visits, lab draws, and ultrasounds. When appropriate, we may conduct visits over the phone or by video. Our nutritionist and wellness appointments can be completed by phone and video. You may want to consider obtaining a scale and blood pressure cuff so you may monitor your weight and blood pressure at home. We will continue to be available in the office for key appointments and for any problems that may arise.
Can I still take childbirth education classes during the COVID-19 pandemic?
Yes, and we encourage you to take this time to gain as much information as you can. Our childbirth educators can host virtual childbirth classes and free online classes. Availability will depend upon the number of families who are interested. Please call 802-371-5901 to inquire about options and availability.
Should I have induced labor due to the COVID-19 pandemic?
At this point, we are not changing our approach to induction. We do not feel that it is safe to induce labor prior to 39 weeks of gestation unless there is a medical reason to do so, such as high blood pressure, or if the baby is not growing well.
After 39 weeks, you and your provider may decide to induce or await spontaneous labor. We are happy to discuss the options with you and the different approaches you may want to consider.
Should I have a home birth due to the COVID-19 pandemic?
It is important to note that having an out-of-hospital birth will not eliminate your risk of exposure, as COVID-19 is now spreading by community transmission.
Here at CVMC, we are working every day to protect the health and well-being of our patients, their families, our staff, and our community during these challenging times.
- We have limited routine traffic in and out of the hospital by making temporary changes to our visitation policy.
- We are screening all patients, staff, and visitors upon entry.
- We are regularly sanitizing surfaces and equipment throughout our facilities, and using additional precautions to limit spread of infectious disease.
As you think about where to give birth, it is also important to consider your medical history, and your own plans for things like pain management. Keep in mind, unexpected things can happen even in low-risk births.
While each woman has the right to make her own medically informed decision about where to give birth, the American College of Obstetricians and Gynecologists (ACOG) maintains that hospitals and accredited birth centers are the safest settings.
Click here to view the ACOG Committee Opinion on Planned Home Birth.
Will I need a C-section due to the COVID-19 pandemic?
The indications for cesarean birth have not changed due to this pandemic. If you are actively sick or infected, you may have a higher risk of needing a cesarean, which highlight the importance of physical distancing to avoid infection, especially toward the end of pregnancy. Otherwise, our goal is for a healthy vaginal birth for the majority of women.
What should I do if I am pregnant and I think I have been exposed to COVID-19?
You should self-quarantine for two weeks and contact the CVMC Women's Health team
If you are under self-quarantine, you should not come to the office or hospital for routine appointments. However, if you need urgent medical or obstetric evaluation, we will see you. We ask that you call ahead at 802-371-5961 so we may prepare with appropriate precautions for your visit.
Will COVID-19 hurt my fetus or unborn baby?
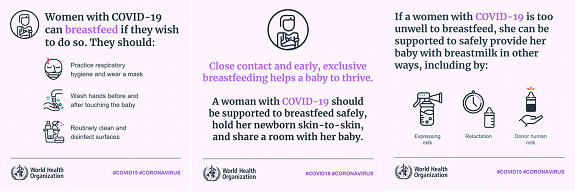
It does not seem that COVID-19 passes through the placenta or breast milk. However, having a fever or getting very sick during pregnancy can cause preterm birth and other complications. As the COVID-19 is a new virus, we don’t yet know the effects of COVID-19 illness during the first and second trimester.
As we learn more, we will update this page with additional information.
Will I be separated from my baby if I get COVID-19?
There is not an easy yes or no answer to this question. We hope that you are not sick with COVID-19 when you give birth. If you are, we will help you make the best decision at the time.
Please understand that NO ONE wants to unnecessarily separate newborns from their mothers, or from any care provider. While we don’t think infants are at higher risk for contracting COVID-19, the truth is we do not know for sure. That said, we do know that infants are generally very vulnerable to any kind of infection.
Therefore, best thing that a pregnant mom can do to protect her infant from COVID-19 is to avoid exposure to the virus herself. This highlights the critical importance of strictly following social distancing practices:
- Get vaccinated.
- Stay at home as much as possible.
- Do not invite people into your home.
- Do not go out unless the trip is essential.
- Do not work outside the home after you are 37 weeks pregnant.
- Keep your children at home as much as possible.
- Do not arrange play dates or other group activities.
- Use technology and social media to keep in touch.
- If you must go out to work or the grocery store:
- Keep a distance of 6 feet from others at all times
- Use hand sanitizer
- Avoid touching public surfaces
- Don’t touch your face
- Wash your hands when you get home with soap and water for at least 20 seconds.
Unfortunately, a pregnant woman may do all the right things and still come down with COVID-19. If you are sick at the time of delivery, we will have to think carefully about whether to separate mom and baby.
Studies show that the virus does not pass through the placenta or breast milk. However, once mom and baby are breathing the same air, the virus may pass via small droplets in the air.
Below are some things to consider as we weigh whether to isolate a newborn from a mother who has COVID-19.
Benefits of skin-to-skin mother/infant contact | Benefits of separating mother and baby |
|---|---|
Regulates the baby’s heart rate, temperature, breathing, and oxygen saturation, helping them to better adapt to life outside the womb | Protects infant from transmission of virus and ensuing illness |
Following a period of skin-to-skin contact, milk volume increases and the milk will contain the most up-to-date antibodies | Protects infant from further medical procedures and interventions that would be required in the face of febrile illness |
Stimulates the release of hormones to support breastfeeding and mothering | Reduces chance that infant may pass virus to other family members or caregivers |
Stimulates digestion and an interest in feeding |
|
Calms and relaxes both mother and baby |
|
Enables colonization of the baby’s skin with the mother’s friendly bacteria, thus providing protection against infection |
|
Experts disagree on whether the right approach is to keep moms and babies together, or to isolate them in the cases where the mother is known or suspected to have COVID-19.
We want to help you make the best decision for you and your family. This decision may depend on several factors: your own values and beliefs, how sick you are, whether you are at home or in the hospital, your ability to keep up with strict hygiene, and the availability of other family members to help care for your infant.
Regardless of whether you are practicing skin-to-skin or physical separation, we want to support your ability to feed your baby your breast milk, which has antibodies and other properties that may be even more critical at this time.
Can I use nitrous oxide in labor? What pain control options are available?
At this time, with the guidance of our professional organizations, we have suspended our nitrous oxide program, as there is not enough information regarding its safe use amidst the COVID-19 pandemic. Specifically, there are concerns related to aerosolization of the COVID-19 virus when using the nitrous system, especially in patients who may have the virus without showing symptoms yet.
Our first priority is patient and staff safety. Therefore, we are utilizing other pain management techniques, including:
- Positioning, movement in labor
- Aroma therapy
- Distraction/relaxation techniques
- Hydrotherapy (labor tubs)
- IV pain medication (Stadol/Morphine)
- Epidural Analgesia
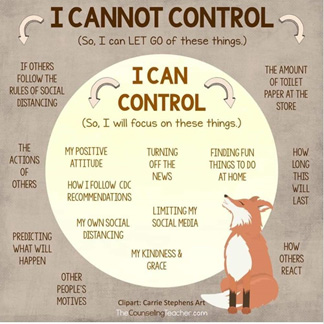
What can I do if I am struggling with anxiety or depression during this time?
We are fortunate to have excellent behavioral health clinicians and counselors available to our patients. If you haven’t already connected with Angela Shea, LICSW, LADC or Hillary Montgomery, MA, LCMHC, LADC, now is a great time to do so. You can set up a free telephone visit with one of them by calling our office at 802-371-5961.
In the meantime, here are some things you can do right now:
(courtesy of NAMI.org)
Breathe Slowly and Deeply
It’s free! A portable tool to use anytime and anywhere. Make sure you inhale through your nose and exhale for longer than you inhale, either through your nose or through pursed lips.
Validate Your Experience
What we are all experiencing now related to COVID-19 is real and scary. There is nothing “wrong” with us. Fear and anxiety are normal responses to abnormal experiences.
Think Positively for 12 Seconds
Bring to mind something positive, such as a beautiful flower, a loved one’s smile, or scenery. And really focus on it for 12 seconds. Breathe and notice its impact on your body and emotions. According to neuropsychologist Dr. Rick Hanson, it only takes 12 seconds for the creation of new neuron connections. These positive experiences have the ability to replace stress/fear based thinking and coping.
How do I stay safe during the COVID-19 pandemic?
Take preventive action to help stop the spread of germs.
- Wash your hands often with soap and water for at least 20 seconds. If soap and water are not available, use an alcohol-based hand sanitizer. Always wash your hands when they are visibly dirty.
- Avoid touching your eyes, nose, and mouth with unwashed hands.
- Cover your coughs and sneezes with your sleeve or a tissue, then throw the tissue in the trash and wash your hands.
- Clean and disinfect frequently touched objects and surfaces using a regular household cleaning spray or wipe.